From the Editor
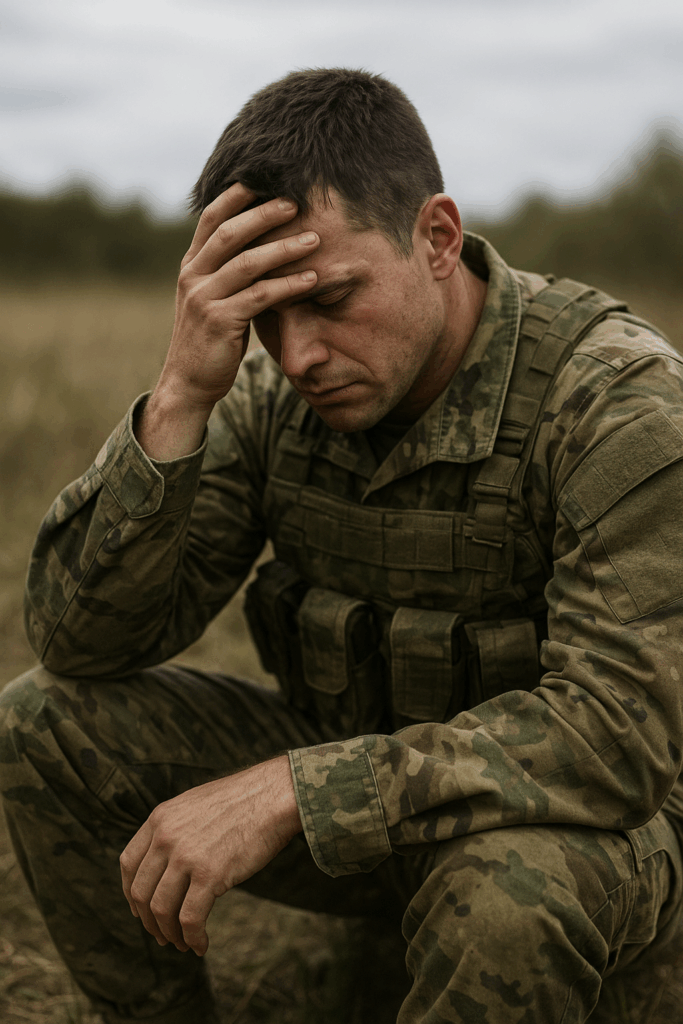
He tried CBT, yet he remained deeply depressed. What should come next? For the record, my patient wasn’t enthusiastic about trying additional medications. Like many, he favoured psychotherapy to antidepressants.
In a new Lancet Psychiatry paper, Thorsten Barnhofer (of the University of Surrey) and his co-authors attempt to shed light on the issue. They report on a randomized, controlled, superiority trial involving 234 participants who had depression and completed a dozen or more sessions of therapy – but remained ill. In the study, these participants received either mindfulness or treatment as usual and were followed for 34 weeks. “Our findings suggest that mindfulness-based treatment can be beneficial after non-remission from major depressive disorder following psychological, stepped care treatment.” We consider the study and its implications.

In the second selection, Yilin Ning (of the National University of Singapore) and her co-authors look at the potential of AI for medical education. In a paper for The Lancet Digital Health, they note great opportunities – particularly as low and middle-income nations face shortages of healthcare providers – but they also describe challenges. “AI offers great promise for enhancing the quality and accessibility of medical education and physician training, from personalised learning experiences to the simulation of complex clinical scenarios.”
Finally, we explore the latest news with articles from The New York Times and The Washington Post. The topics: the case for mandatory treatment, glucagon-like peptide-1 agonists for substance, and the life of Dr. Nolan Williams.
DG







Recent Comments